We respect your privacy.
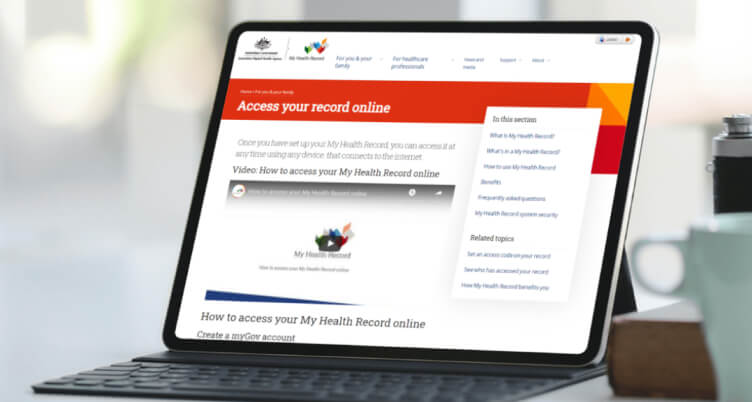
To create a My Health Record, we will collect information about you and your children from Medicare and some other government bodies including your name, date of birth, and Medicare records from the last two years.
Registered healthcare provider organisations such as general practices and hospitals will be able to access your My Health Record when providing healthcare to you.
You can set access controls to restrict which healthcare providers can see your health information.
We don’t disclose your information to anyone else, unless required or permitted by law.
More information can be found at www.myhealthrecord.gov.au/privacy.